What is contact tracing?
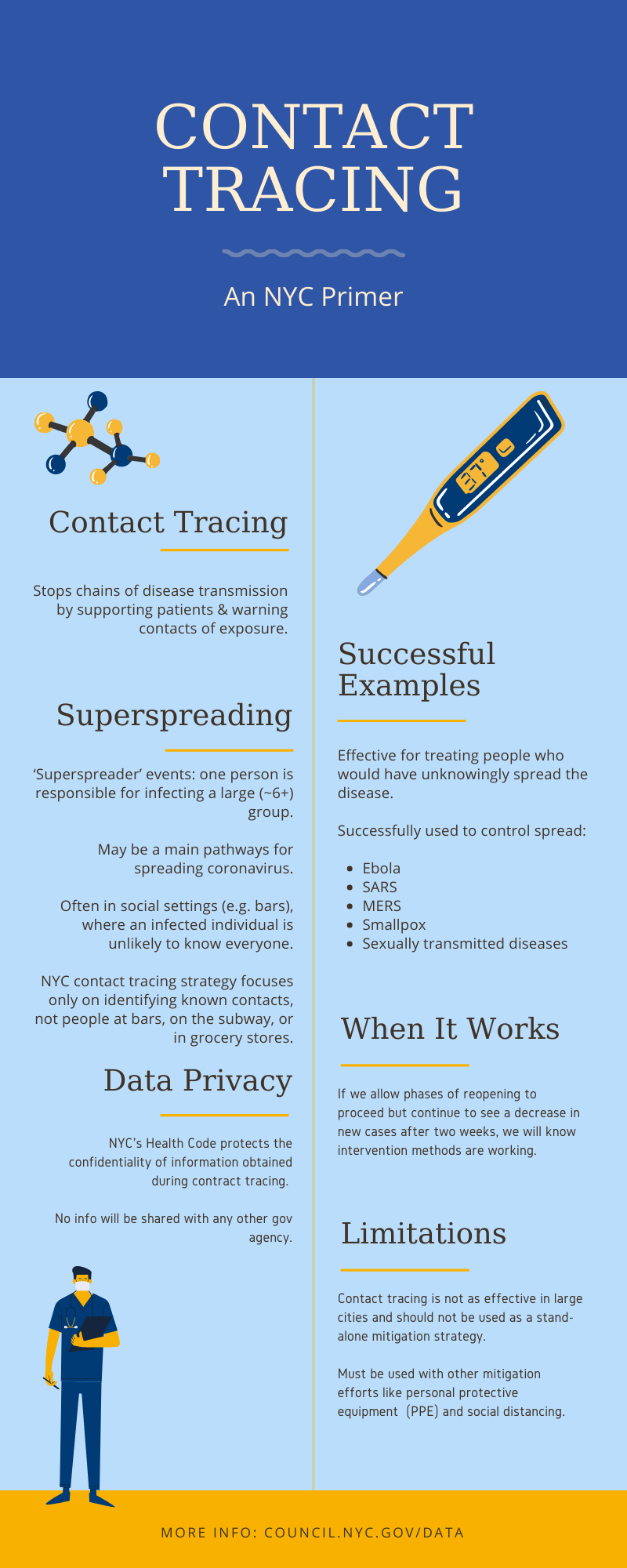
Contact tracing is the process of identifying, assessing, and managing people who have been exposed to a disease to prevent onward transmission. When systematically applied, contact tracing will break the chains of transmission of an infectious disease.
An important component to the success of contact tracing is community engagement. Contact tracers must understand the needs of the community that they are serving, which includes languages spoken, literacy, cultural customs, agency, and stigma.
For contact tracing to be successful, there needs to be cooperation between communities and public health departments. The success of any contact tracing program depends on everyone pitching in to help.
Successful examples
Contact tracing, aka ‘partner notification’, has been successfully used to control the spread of ebola, SARS, MERS, smallpox, and sexually transmitted diseases. In the case of STDs, contact tracing is extremely effective. It is particularly useful for uncovering asymptomatic cases, thus providing a way of treating individuals who would otherwise continue to unknowingly spread the disease.
While there are challenges to tracking a disease that is spread via airborne respiratory droplets, this same principle can also be applied to Covid-19. Contact tracing can identify individuals before they show symptoms (pre-symptomatic) or asymptomatic individuals who may be unknowingly spreading the infection.
Conditions for Success
Contact tracing is effective when we have:
- Enough staff from the target communities to reach out to everyone who is sick
- The number of cases is low enough that you can trace and reach all contacts
- People contacted listen to recommendations

Contact Tracing Process
Contact tracing in NYC is run by Health and Hospitals (H+H) as part of NYC’s Test and Trace Corps.
As of Oct. 19 the Corps employed 3585 contact tracers and community engagement specialists.
Every person who is identified as sick is put in touch with a contact tracer. The contact tracer then works to identify their contacts and ensure they have the resources they need to remain isolated while carrying the disease.
Why it works
Preventing this scenario will require a number of different measures like maintaining social distancing, wearing masks, and washing hands. Contact tracing also plays a key part. If we allow certain phases of reopening to proceed but continue to see a decrease in the number of new cases after two weeks (the approximate lag between infection and hospitalization), we will know intervention methods are working.
COVID-19 is particularly difficult to contain because those infected go through a pre-symptomatic period in which they show no visible signs of infection but are still contagious. Best medical research suggests that the average individual will become symptomatic approximately 5 daysafter infection. However, there is some evidence that individuals become infectious (able to infect others) around 3 days after infection. Individuals may also be the most infectious before or right when they begin to show symptoms
Effective contact tracing can allow us to identify these pre-symptomatic individuals while they are still infectious and before they show symptoms. Identifying these cases and ensuring they have the required services to isolate will help stop the spread of COVID-19.
COVID-19 also appears to have a high fraction of infected individuals who never show symptoms – in other words, asymptomatic infections. Proper contact tracing can help ensure these individuals are identified even though they don’t feel sick, thereby preventing them from spreading the virus indiscriminately.
There are a few metrics used to measure the success of a contact tracing program. These include the proportion of contacts reached (given by cases that had contacts). Ideally, all cases would have no contacts or few contacts, because the program would be supplemented by social distancing measures, and contacts would be caught quickly enough that they didn’t have the opportunity to spread the infection.
As contact tracing becomes more robust and effective, the proportion of cases who were contacts themselves increases. This indicates that the program is effectively controlling spread.
Other simple metrics of success include:
- Percentage of cases that were contacted within 24 hours of case report
- Percentage of contacts that were notified and quarantined within 24 hours of outreach
All of this success requires community buy-in. According to Resolve to Save Lives, an initiative of Vital Strategies led by the former head of the CDC and DOHMH, Dr. Tom Frieden, communication with the public is one of the key factors in a successful test and trace program.
Superspreading
There is some evidence to suggest that ‘superspreader’ events, where one individual with many contacts is responsible for infecting a large (~6+) group of others, may be one of the main pathways for spreading coronavirus.
Superspreader events are much more likely to occur in places where lots of people gather.
person infected between 32 and 52 other individuals.
These concerns are why New York State guidelines require one member of each party eating at a restaurant indoors to leave their contact information for the purpose of helping with contact tracing efforts.
In addition, this requirement is just one of many, such as keeping density at indoor restaurants at 25% capacity and requiring diners to wear face masks when not eating, that all attempt to prevent the spread of infection indoors
Local Law 61
New York City Local Law 61 requires that Health+Hospitals report weekly and eventually daily on which communities are being served by NYC’s Test & Trace program.
H+H is required to report on the number of contact tracers employed by languages spoken and zip code of residence.
In addition, H+H is required to report on the number of cases and contacts disaggregated by “zip code, race, ethnicity, gender, age range, whether they tested positive for currently having COVID-19 or experienced COVID-19 symptoms within the last 14 days, … and whether such individuals were referred to wraparound services”.
Providing this data will allow community-based organizations (CBOs) and researchers to easily identify communities at risk of a spike in COVID-19 cases and ensure that the Test & Trace program is appropriately meeting the needs of the city’s vulnerable communities.
Exposure notification apps
Exposure notification apps, such as the recently launched “COVID Alert NY” complement traditional contact tracing efforts.
The app does not track your location but instead alerts you to potential exposure by exchanging random codes with devices that were less than 6 feet away from you for more than 10 minutes via bluetooth technology.
Every day the app checks the random codes it has stored against a list of codes identified with the phones of individuals who have tested positive.
If there is a match the app will notify you that you have potentially been exposed to COVID-19 and direct you to take appropriate precautions (quarantining, contacting a medical professional etc.).
Data privacy
The New York City Department of Health & Mental Hygiene has used contact tracing for past outbreaks with a proven record of confidentiality.
Takeaways
- Contact tracing is an essential component of a suite of non-pharmaceutical interventions that will help curtail the spread of COVID-19 within NYC.
- All components are currently necessary to keep case counts low.
- Contact tracing can only succeed with effective community engagement
For feedback, comments, and questions please email Data@council.nyc.gov.
Created by the NYC Council Data Team.